
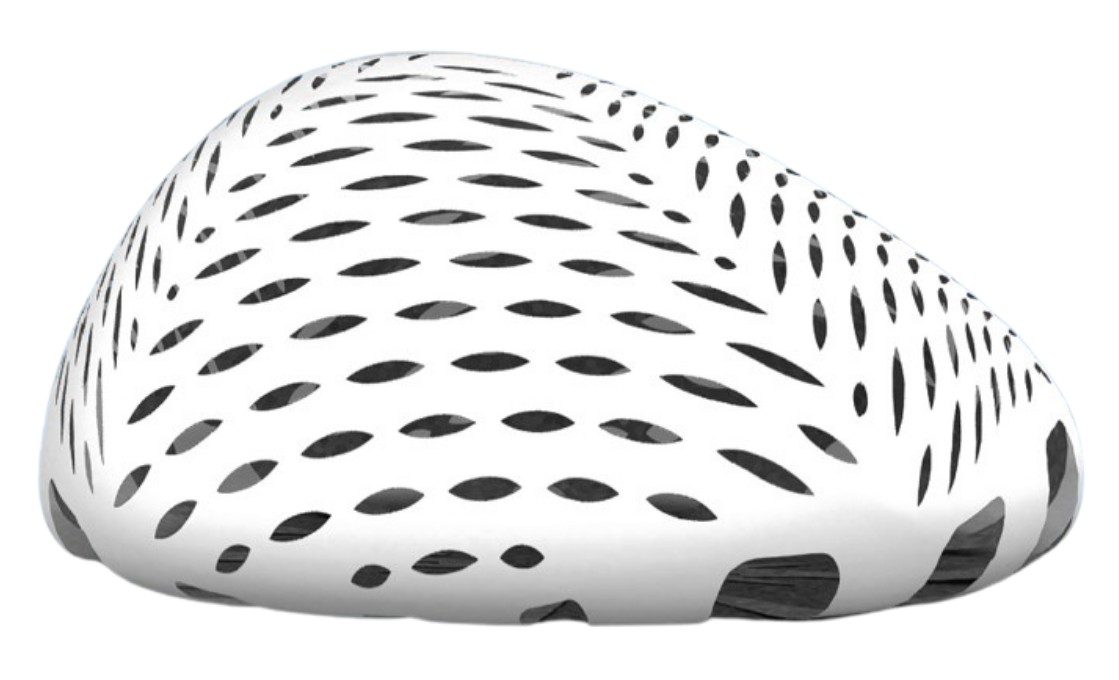
Designed for Reconstructive Plastic Surgery, the Exashape membrane is processed through a proprietary method that maintains the unique qualities of natural bovine pericardium¹.
Exashape Bioshield pocket guarantees fast integration times with cell ingrowth², minimal inflammation³ and negligible serum production, while maintaining remarkable mechanical properties¹.
The two layers perform a specific task in the integration process.
Fibrous layer: highly porous, it welcomes cells and, together with the matrix components, allows cytokines and growth factors to trigger the immediate revitalization process and early neoangiogenesis [2].
Compact layer: it is quickly repopulated by fibroblasts and VEGF². After implantation, there is no accumulation of inflammatory or giant cells. It is the part that provides the most solid structural support.
The bilayer membrane undergoes a 3-stage process of revitalization by endogenous connective tissue.
During implantation, the collagen matrix absorbs the blood and the revitalization process begins immediately, characterized by a controlled and short-lived inflammation phase with considerable neoformation of vessels [2,3].
Fibroblasts reactivate collagen by triggering the ingrowth of new vessels, which provide the metabolic needs. At this stage of the reparative process, cell proliferation prevails, which targets the growth of new tissue [2].
The actual remodeling phase begins its course and is the result of the precise balance in the synthesis of collagen, which becomes an integral part of the tissue [3].
The cell-friendly process preserves the active elements in the repair process within the membrane: proteoglycans, hyaluronic acid, fibronectin, elastin and of course, native collagen. They represent a natural reservoir of bioactive factors, which participate in the revitalization process by controlling inflammation while promoting cell proliferation and migration [2]. We limit the amount of biological mass implanted (up to 50% less, due to lower thickness of pericardium compared to dermis) promoting integration even in cases of poor blood supply, while maintaining the highest bio-mechanical performance [1,4].


REFERENCES